Non-invasive ventilation for children on the ICU

Partner: Amsterdam UMC & nSize
Motivation
In the Netherlands, in addition to the well-known adult ICUs, there are also seven Intensive Care (ICU) departments for children (NICUs). More than half of the children in the NICU need a ventilator because they have severe – or even life-threatening – shortness of breath. Often a breathing tube is inserted through the throat for this and a child is then so-called “invasive ventilation”. However, this type of ventilation has many adverse side effects, such as infections and long-term lung damage. Also, these children often have to be kept asleep for a long time. For these reasons, the use of non-invasive ventilation (NIV) has increased significantly over the past two decades. With NIV, a child is ventilated through a mask on the face. This provides many benefits, but the effectiveness of the ventilation is highly dependent on the fit of the mask. Particularly for young children, few shapes and sizes are commercially available.
Also in the NICU of the Amsterdam UMC, children are – for lack of better – ventilated with masks that do not fit properly. Jip Spijker’s graduation project titled “Tailored non-invasive ventilation masks for pediatric intensive care” has yielded two design options for a mask that ‘fits better’, which optimizes ventilation (Spijker, 2020). For long-term ventilation, a (modular) mask has been designed that is custom-made, for example by means of 3D printing. The properties and adaptations that are necessary for an optimal fit on an individual child’s face and the process to get there are further investigated in this project.

Problem definition
Little is known about the variation in children’s faces, especially at a young age. There is also no existing way to personalize breathing masks within a short period of time (24 hours) on an individual child’s face. The aim of this Fieldlab UPPS project was to make personalized respiratory masks for children, in order to provide better treatment with NIV in the Pediatric ICU. We specifically looked at the possibilities of making these types of masks using 3D scanning and printing. We investigated this based on the following research question:
“What is the process leading to the production of the ideal, custom-made mouth-nose mask for infant respiration (0-7 years) for long-term use, initially for hospital application within a target period of 24 hours? ”
Activities & task distribution
In total, three parties were involved in the project, namely: Amsterdam UMC, nSize and the Fieldlab team. The project is led by Renee Hovenier, a Technical Medicine graduation student at Amsterdam UMC.
To achieve the goal, the project is divided into five parts. In the beginning, the basic design, based on that of Jip Spijker, was finalized and the final shape, basic dimensions, material and production were determined. Subsequently, nSize created a parametric model that can load an individual scan of a child’s face and allow the mask to fit seamlessly on the child’s face using manually placed ‘landmarks’. In order to be able to test the mouth-nose masks, two test heads have been developed. Pressure sensors were used to get more information about the pressure of a mask on the face. Finally, the process from scan to use was mapped and optimized by the Amsterdam UMC.
Results and conclusions
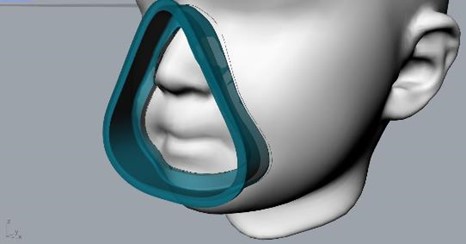
As a result of the project, there is a detailed basic design of the mask, which features two standardized parts (3 and 5) available in 6 sizes and the soft, custom-made ‘cushion’ part (4).
An extensive material study has ultimately resulted in the basic design with suitable material choice (MED610 and MED625FLEX), which are biocompatible, transparent and suitable for medical application. The transparency is crucial to be able to see any blood or vomit. In addition, the material can be worn on the skin for prolonged periods of time. The flexibility (Shore value) of the ‘cushion’ part is also important for a seamless fit on the child’s face. Ultimately, two full prototypes were developed with these materials, printed with the Stratasys J35 Pro.
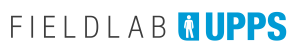
The algorithm to come from 3D scan to a printable version of the personalized ‘cushion’ is made as a plugin for the program Rhino (Rhinoceros 7, McNeel, Miami), which can be downloaded and used with a license. An enclosed manual also explains all (installation) steps and provides guidelines for using the software.
In the development process, two test heads were developed to test the prototype mouth-nose masks. These test heads are made up of a hard inner surface surrounded by a soft, silicone layer that mimics the skin. Channels through the nostrils and mouth allow the test heads to be connected to a lung simulator and simulate realistic ventilation. During the tests at the Children’s ICU in Amsterdam, it appeared that the test heads can be properly ventilated and can therefore provide valuable information. Since the heads differ in age (1 year and 4 years), it was possible to also test two sizes of masks (2 and 4 sizes, respectively). The pressure of the mask on the skin was also measured.

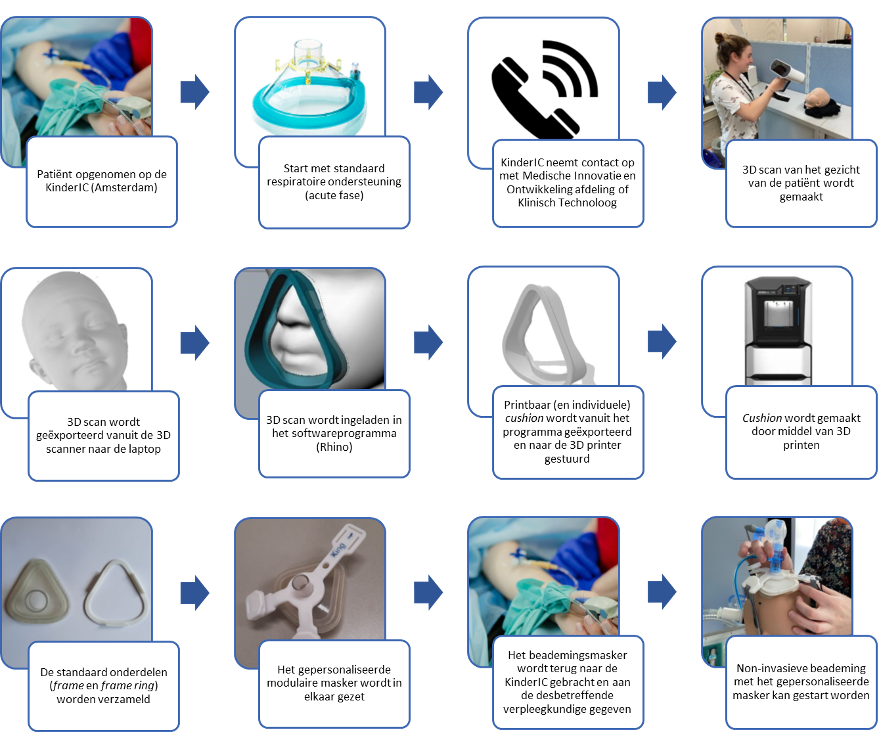
Finally, a process was developed for making the mask for an inpatient in the NICU.